Many thanks to our SoCo Public Health Officer, Dr. Sundari Mase and our SoCo Vaccine Chief, Dr. Urmila Shende for an excellent Grand Rounds this week on Pandemic Pearls and Pivots: A Public Health Perspective.
A recording of their presentation is available HERE.
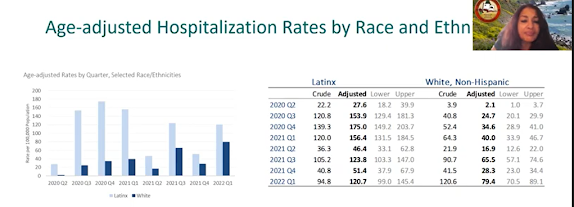
As we all know, COVID-19 has taken a great toll on our world, our nation, and our county. As of this week, there have been 6.28 million deaths worldwide (probably an underestimate), >1 million US deaths (more have died from COVID-19 than HIV/AIDS, the 1918 influenza pandemic), 90,000 deaths in California, and 491 deaths in Sonoma County. This has led to the largest drop in life expectancy since WWII. And we know that there have been disproportionate numbers of cases, hospitalizations, and death among people of color.
- Building Public Health testing capacity
- SoCo regional lab has done 206,000 (of 1.6 million PCRs total) to date in SoCo
- State of California and FQHC partnerships
- Focus on equity
- bilingual messaging
- pop up testing sites (using local data to determine neighborhoods for sites)
- bilingual/bicultural testing/contact tracing
- With increase in Ag testing (no longer have a denominator), we are beginning to pivot toward wastewater surveillance
- Communication campaigns, outreach, press conferences
- re. masking, hygiene, social distancing, gathering size limitations
- reaching so many different sectors, subgroups was VERY challenging (e.g. reaching the elderly: age, transportation, low tech)
- local radio, social media: FB, instagram, etc, flyers
- work with community based organizations, promotoras essential
- Shelter in place (averted huge surge/disaster early on)
- Alternate care site/non-congregate site (for people with unstable housing, served thousands of people, SSU>>hotels)
- State, local and Bay Area health orders to protect vulnerable populations
- Vaccines
- Magnification of underlying/pre-existing disparities
- Latinx residents: largely essential workers, hardest hit
- 27% of our population is Latinx, accounted 45% of all cases
- at one point, case rate was 9X higher for Latinx
- In 2020, life expectancy decreased by 2.1 years in Latinx population (compared to 0.7 years in White SoCo population)
- Addressing these inequities, THE PUBLIC HEALTH CHALLENGE of this pandemic
- Health Equity Working Group helped get services to vulnerable population
- trusted messengers (community health workers, promotoras)
- vaccines, masks/PPE, rental assistance
- CURA: important partner to reach community, ensuring financial assistance provided to people who needed it ($8 million)
- FQHC network for collaboration--> 13 different vaccine sites to prioritized populations
- Special shoutout to Dr. Jenny Fish and Dr. Panna Lossy for uplifting the voices of vulnerable communities
- 75% of SoCo deaths were in people >65
- residents of skilled nursing facilities were particularly vulnerable prior to the introduction of vaccines
- SoCo PH chose to prioritize the most vulnerable residents for vaccine roll out
- older adults (65+, 75+)
- SNF and residential care facility patients (RCF)
- Essential workers and marginalized communities (health workers, farm workers, food service workers, homeless)
- We have very high degree of vaccination in our elders: 93% of those >65 are fully vaccinated
- Vaccination of vulnerable elders reduced deaths at SNFs and RCFs
Vaccines work! The reduce infection, hospitalization, and deaths.
 |
| from https://socoemergency.org/ |