A recording of the presentation is available HERE.
***
Many thanks to Dr. Erin Felton for an excellent presentation on a hot topic: GLP-1 Receptor Agonists, the class of medications that is literally taking our nation by storm. As Dr. Felton said during her presentation, direct to patient advertising and word of mouth has led to droves of patients coming to their providers asking for these medications, most commonly, for weight loss.
A recording is available above.
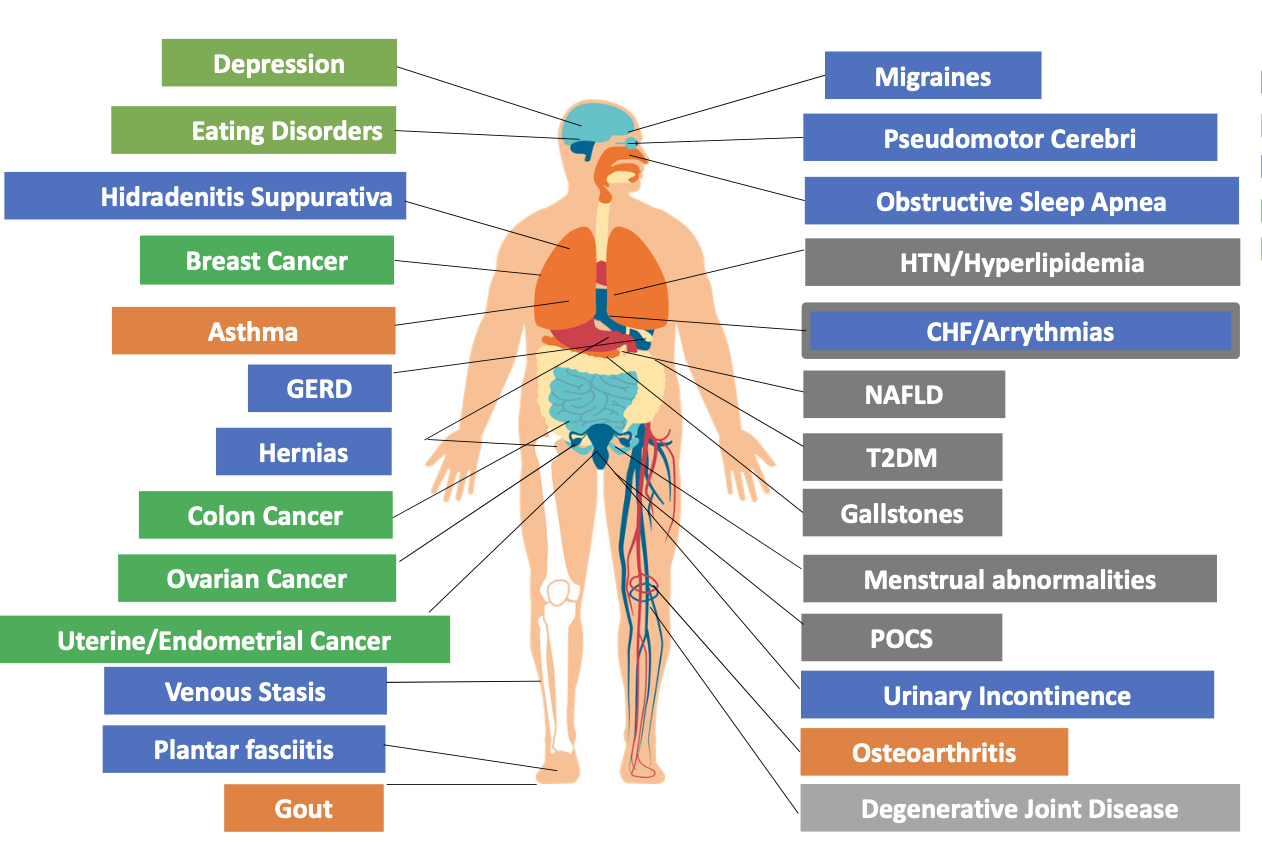 |
| comorbidities associated w/obesity |
Here are my notes:
- obesity is a chronic, relapsing , treatable multifactorial disease
- it is associated with comorbidities (e.g. HF, DM2, uterine cancer) and complications
- BMI, as we know, is not a perfect measure, but it's what we currently have
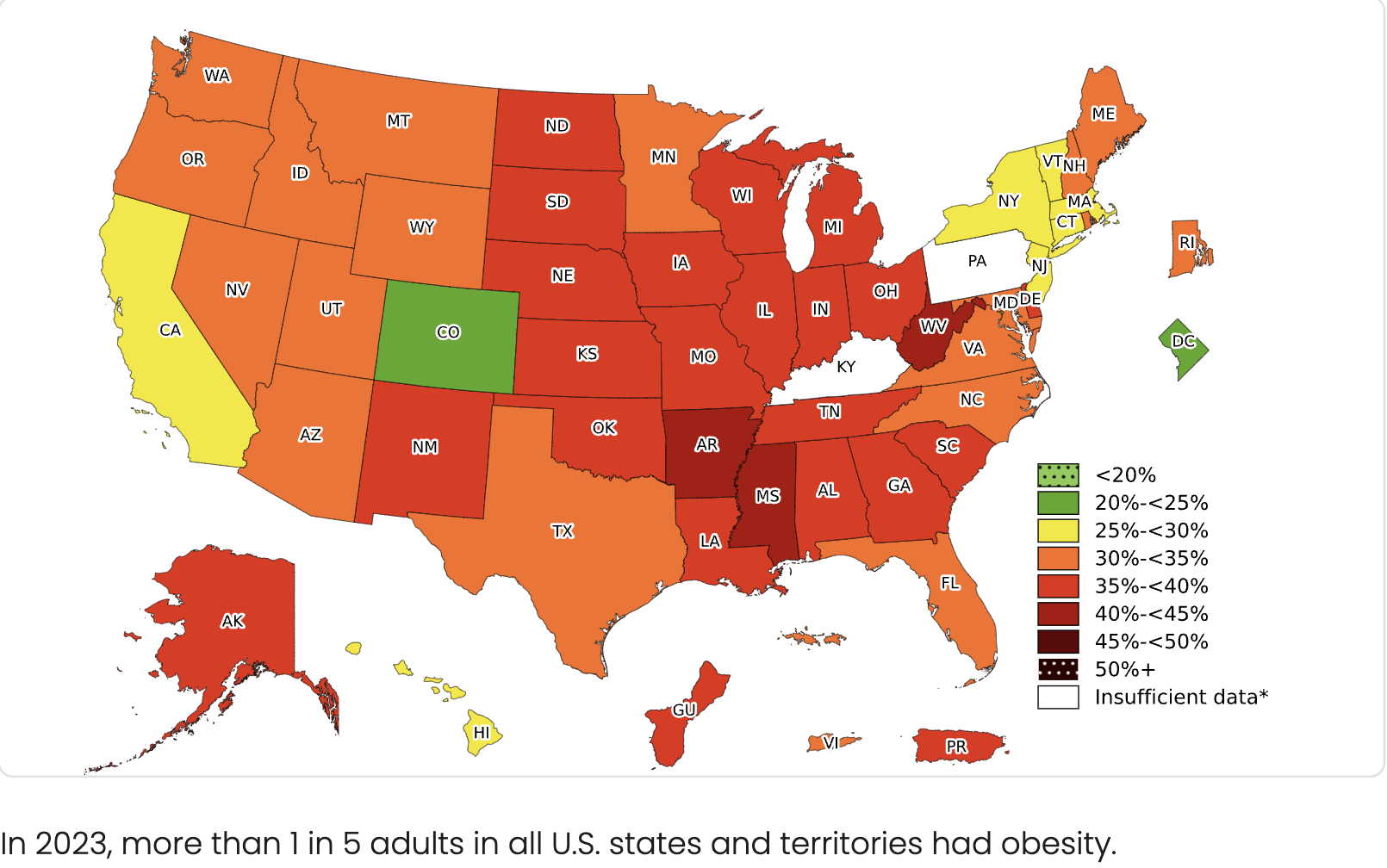
- According to 2023 CDC data: 1/5 US adults are obese
- By 2030, there are estimates that 1/3 US adults will have a BMI>30
- There are racial and socioeconomic disparities associated with obesity
- these are particularly evident in communities of color (black and Latinx)
We must be aware of our own "fat bias" in medicine
- always ask patients for permission before discussing their weight
- give patients a right to decline weighing in
- focus on chronic disease aspect of obesity (rather than weight)
- consider how to create a supportive environment for obese patients
There are several FDA approved medications for obesity, the GLP-1 Receptor Agonists are the new kids on the block, but see the image below for all meds that are currently approved for long-term usage, short-term usage, and off label usage:
GLP-1 is an endogenous incretin hormone that is produced by the L cells in the distal ileum and colon in response to food intake. GLP-1 receptor agonists mimic this mechanism. In addition, GLP-1 receptors are expressed in multiple organs: GI tract, pancreas, hypothalamus, brainstem, heart, kidney, muscle, fat cells. It is thought that effects on the brain influence appetite and satiety. Receptors in the GI tract decrease gastric emptying and slow gastric motility.
Current GLP-1 Receptor Agonists:
 |
Murphy EJ,”What’s new in Endocrinology”, Medical Management of HIV Conference, 2024
|
The newer kid on the block are multi-targeted incretin therapies, including GIP, which is secreted more proximally in the small intestine; it stimulates downstream GLP-1, enhances insulin, promotes satiety and seems to be associated with less nausea.
The newest agent, tirzepatide, is a combo of GIP/GLP-1. There are currently two versions of tirzepatide on the market: Mounjaro (indication: DM) and Zepbound (indication: weight loss). Zepbound is currently covered by Partnership medi-cal.
Current combos/multi-targeted incretin therapies:
Specific prescribing info for semaglutide and tirzepatide:
There are no direct head to head trials comparing semaglutide to tirzepatide.
Indirect comparisons suggest more weight loss with tirzepatide, as well as potentially lower side effect profile.
Side Effects
We should definitely be talking to our patients about side effects when we are prescribing these medications.
The most common side effects of GLP-1 medications are GI symptoms (nausea, vomiting, constipation, etc). GI symptoms are extremely common (25-40%) but do decrease over time. In many trials, a large percentage of people self-discontinued the medications due to side effects.
Going slow can mitigate the GI side effects, as they do abate over time. Reducing meal size and adopting a low fat (and low glycemic index) diet can also reduce side effects. Patients should have some nutritional counseling (even if it's just from the PCP). Increasing fiber may also help.
Dizziness and dehydration have also been reported. This could be due to morning hypoglycemia. Small frequent meals and maintaining good hydration are recommended.
As mentioned above, the newer combination medications MAY be better tolerated.
Contraindications to these medications include: medullary thyroid cancer/MEN2, pregnancy, hx pancreatitis or gallstone disease (relative/not absolute). Of note, there was some post-marketing signal in 2023 suggesting a correlation with suicidality, further assessment in 2024 did not confirm this signal, but consider ongoing assessment in patients with a hx of depression or SI.
Starting/stopping
There is good evidence that discontinuing GLP-1 meds lead to gaining back a large percentage of weight that was lost (though overall, pts do maintain a small percentage of weight lost). A retrospective cohort study of 125K patients, just released in 2025 found that 53% of patients and 72% of patients had discontinued these medications at 1 and 2 years, respectively. Somewhere between 1/3 and 1/2 of these patients resumed these medications within 1 year of stopping.
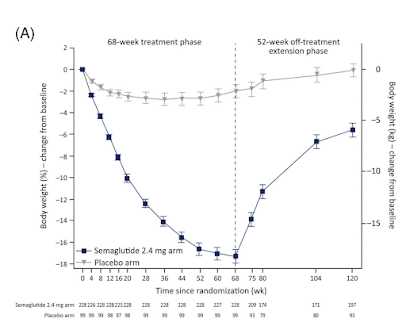 |
| Wilding et al, Step 1 Extension, Diabetes Obes Metab 2022 |
About insurance:
- Medicare specifically does NOT cover weight-loss drugs. However, as of 3/24, Medicare will cover semaglutide for obese patients for CVD prevention IF they have documented CVD (e.g. prior MI, PVD, etc)
- Only about 20% of Medicaid programs cover weight loss drugs (Medi-Cal does! See the image below showing the current PHP covered medications)
- Only about 25% of employer-based insurance cover weight loss drugs
- Locally, Kaiser does NOT cover weight-loss drugs unless you have another specific indication (e.g. DM2, HFrEF, CVD)
- There has been varying pharmacy supply
Patient Counseling pearls
- There is significant weight regain after discontinuation of GLP1s, though studies so far have still showed a net loss.
- Most patients who newly initiate treatment with GLP RA discontinue within 2 years.
- High burden of GI side effects, gets better with time.
- Need for long term therapy due to weight regain?
- Other factors for adherence: high cost, availability of medication
- All studies done at target dose of 2.4mg
Finally, there are more and more studies being published showing benefit in outcomes other than weight loss. These include CVD, OSA, MASN/MAFLD, dementia, Parkinson's, disease, as well as substance use disorder. Stay tuned.







