Many thanks to Dr. Tiffani Strickland, who gave an action packed Grand Rounds this week on Treating Opioid Use Disorder in the Hospital. She covered a ton of ground on this important topic-- from opioid use trends to adverse child experiences to trauma informed care to micro-dosing of buprenorphine in the hospital.
To see a full recording of Dr. Strickland's excellent presentation click HERE.
My notes:
- Overdose deaths from opioids are off the charts and continue to increase in the US and in our own Sonoma County (see graphs below, including local data)
- If you only have 5 minutes, watch this video about our current understanding of addiction and social isolation: "Everything you know about addiction is wrong". It challenges our traditional framework for addiction and substance use disorder.
- Also consider reading this book: Chasing the Scream (by Johann Hari)
| SoCo DPH opioid overdose rates (Death and ED visits) |
Racism and the opioid epidemic

- Despite similar rates of drug use, Black Americans (who make up 13% of the population) make up 27% of drug arrests (2018)
- Disparities in incarceration have affected generations of communities of color
- African American and Hispanic Americans are 7.5 and 2.3 times more likely to have an incarcerated parent (than white children)
- having an incarcerated parent puts children at increased risk for future substance use
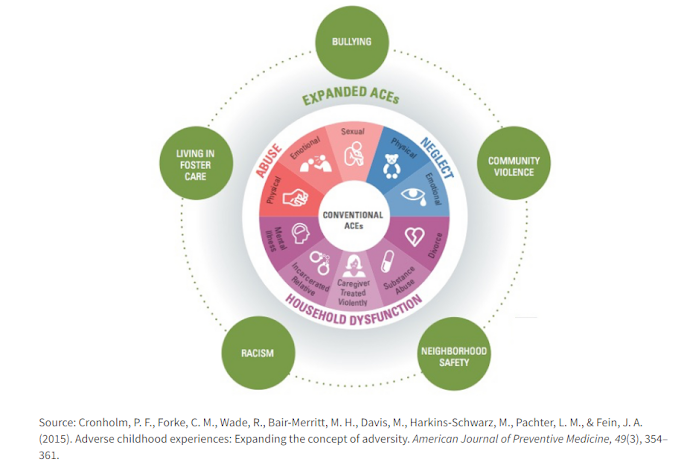
Adverse Childhood Events (ACES)
We know that ACES (childhood abuse, neglect and household dysfunction)are associated with risk for substance use disorder. I.e. the more ACES you have, the higher risk you have to have issues with substances, including IVDU.
Trauma Informed Care
- It is our job to care for patients with a hx of trauma by influencing healthy coping mechanisms and helping patients build resiliency
- The Substance Abuse and Mental Health Service Administration (SAMSHA) decribes 6 principles of a trauma-informed approach. These are SO important to consider in how to engage with all patients, but particularly those with high ACE scores
- Safety
- Trustworthiness and transparency
- Peer support
- Collaboration and mutuality
- Empowerment, voice and control
- Cultural, historical and gender issues
- Again, providers should consider how to help patients focus on RESILIENCE and COPING
- Examples of how to do this include
- Openly discussing harm reduction methods (prevent dying and suffering)
- Person first language, welcoming, non-discriminatory, non stigmatizing language
- i.e. person with substance use disorder, person in recovery
- i.e. avoid "clean" and "dirty" when talking about drug screen results
- Put up signage offering treatment for opioid use disorder in hospitals and clinics
Words Matter! Check out these tables to make sure that you are using language that is non-stigmatizing.
https://www.drugabuse.gov/sites/default/files/nidamed_wordsmatter3_508.pdf |
Treatment of acute pain and management of withdrawal
- If a patient is on BUP, don't STOP it when treating acute pain
- patients can safely get acute pain meds on top of their BUP
- you will only precipitate withdrawal at initiation of BUP
- split dosing to BID for pain management in the acute setting
- provide sense of calm and comfort (help patient feel safe and connected)
- Also, schedule tylenol and/or ibuprofen (or toradol) in setting of acute pain
- consider gabapentinoids, SSRI, TCA, regional block
- can increase up to 32 mg/day for acute pain
- add opioids with higher Mu affinity: morphine, hydromorphone, fentanyl
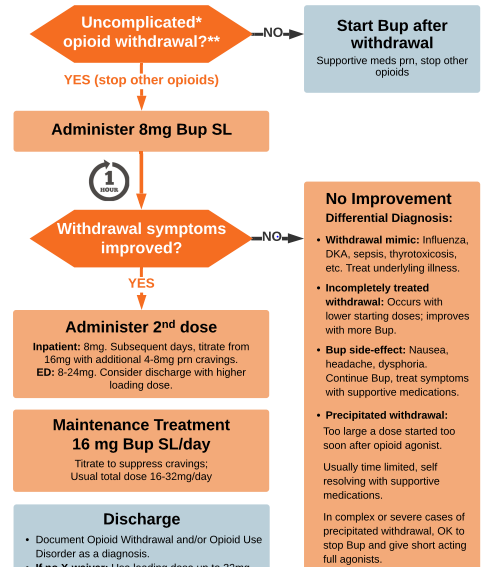
- Very simple! For uncomplicated withdrawal (COWS>8), start with 8mg BUP SL, recheck in 1 hour, give second dose of 8mg
- Subsequent days, titrate from 16mg with additional 4-8mg prn cravings
- Labs to consider (but don't need results to start): UDOA, CBC, HIV, HCV, RPR, HCG, HAV and HBV immunity
- Adjunctive medications: acetaminophen (pain, headache), clonidine (w/d symptoms), diphenhydramine (anxiety), loperamide (diarrhea), ondansetron (n/v), trazodone, melatonin (sleep)
Microdose inductions of BUP
- Very slow start of BUP to decrease or even eliminate withdrawal symptoms
- Consider: if patient taking methadone, history difficulty BUP start, transitioning from prescription opioids, intentionally taking fentanyl daily
- Avoid: if already significant withdrawal (it's too slow), don't want to continue full opiate agonist, risk for respiratory depression/sedation, prefer rapid start
Harm reduction refers to a set of policies, programs and practices that aim to reduce health, social and economic consequences of drug and alcohol use.
- Reduce stigma by being a safe place, regardless of ongoing substance use
- Offer clean needles (available at Face to Face, DAAC, but also on PHP formulary (see image below)
- Always give Narcan Rx
- Give Fentanyl test strips (available at Face to Face)
- Resource support
- If patient leaving AMA, give direct phone # to outpatient MAT care:
- Marla Pfohl MAT program manager SRCH 707-890-0375
- Erick Hill, Matt Clinic supervisor SRCH 707-867-8690
- Never Use Alone phone # 800-484-3731
- Connect to outpatient MAT, give bridge Rx to outpatient MAT (x-license no longer required)




This comment has been removed by a blog administrator.
ReplyDeleteThis comment has been removed by a blog administrator.
ReplyDeleteThis comment has been removed by a blog administrator.
ReplyDelete