Many thanks to Dr. Janice Manjuck, our SSRRH ICU Director, for an excellent Grand Rounds this week on Oxygen Delivery and BiPAP for hospitalized patients. Dr. Manjuck gave us a nitty gritty review of when/how/why we might select one of many oxygen delivery devices. She combines humor, basic science, and evidence in just the right blend to bring us clinically relevant learning. We are so grateful!
A recording of her presentation is HERE. Feel free to check it out.
My notes:
First, off, when should we be using oxygen?
- if patient is acutely ill, oxygen is not indicated unless saturation is <96% (this excludes sickle cell crisis, CO poisoning, profound anemia (Hb <3) and pneumothorax
- in ACS/CAD aim for 93% saturation
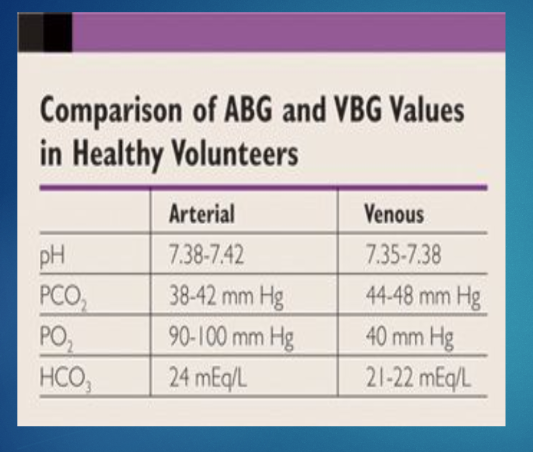
ABG vs. VBG: For patients NOT in shock, a VBG is a relatively good alternative to an ABG, particularly if you are getting the VBG to trend PCO2 in hypercapnic patients. VBGs are easier to get and less painful for patients. However, please note, if a patient is in shock, an ABG may be needed. Do not be offended if the intensivist asks for an ABG for an unstable floor patient!
Okay, when patients need oxygen, what kind of oxygen should I give them? It is important to take into account their clinical status, their comorbidities, and why they need oxygen. Low flow systems, which can deliver 0-15LPM of oxygen, are good for patients with a stable respiratory rate and pattern. High flow systems -- which can deliver 50-60 LPM-- may be better for patients who are more tachypneic.Dr. Manjuck reviewed the concepts of anatomical dead space and entrainment
- Anatomical dead space is the internal volumes of the upper airways, in which no gas exchange takes place -- on average about 150 ML in a 70 kg person. Air is warmed, filtered and humidified in this space, but no gas exchange occurs. So it is essentially "wasted space".
- Entrainment is when room air mixes with oxygen due to a negative pressure gradient. In other words, it is the air that leaks around the oxygen delivery device. This is more common in nasal cannula<<face mask<<HFNC.
- Nasal cannula coming from wall is always delivering 100% oxygen, each 1L/min is equivalent to 3-4% FiO2, remembering that room air contains approximately 21% oxygen, SO
- 1 LPM=24% oxygen
- 2LPM=28% oxygen
- 3LPM=32% oxygen
- 4LPM=36% oxygen
- 5LPM=40% oxygen
- And so on. . .This means that 10 LPM on a nasal cannula gets you about 60% FiO2. See chart .
- A (simple) low flow mask can delivers upwards of 60-70% FiO2 IF the patient is breathing normally (essentially maxed out at 15LPM)
- A non-rebreather mask ALSO gives about 15LPM max of oxygen, which is ~60-70%. It does not flood the face, but rather floods the bag, which is a means to effectively deliver high levels of oxygen anywhere in the hospital. It can deliver 75-90% FiO2, but100% non-rebreather should be considered a fast track to something else (i.e. BiPAP, HFNC or intubation)










No comments:
Post a Comment