Many thanks to Dr. Anne French, who gave us a jam packed 45-minute mini-fellowship in the Care of Patients with Intellectual and Developmental Disorders (IDD) this week. I learned so much! But also am left feeling like I have so much more to learn. Her 11 years of experience as a family doctor at the Sonoma Developmental Center (SDC) and her sharing about her personal care of own brother with Down Syndrome make her an invaluable community resource. If you or someone you know is caring for someone with IDD and needs consultation, keep Dr. French in mind!
Risks: patients with IDD are at higher risk for neglect, abuse, poverty, substandard medical and dental care
- ~46% of patients with IDD are on psychotropic medications
- 3/4 haven't seen a psychiatrist, 1/3 don't have a psychiatric diagnosis
- Many folks with IDD have untreated hearing and/or vision deficits
- High rates of obesity (sedentary lifestyle, poor diet)
- Despite high rates of diabetes and hypertension, most are under-treated and under-screened
- Very high rates of dental caries
| (Dr. French recommends 3 sided toothbrush to prevent caries) |
- learn their language
- "listen with the ears of your heart"
- how do you get a patient to relax in the clinical environment?
- how does illness present differently in this population?
- see them as a fully aware human being
- develop trust
- be willing to abandon your own agenda
- use "people first" language (eg. person with spastic quadriplegia, person with autism)
- understand disability etiquette
- Conservator: the legally appointed person to manage financial, legal, and medical affairs of an adults who is unable to do so (requires $$ and court)
- Consenter: typically family member but also can be a friend (without papers) who demonstrates consistent involvement, recognized in California as valid
- North Bay Regional Center: if there is no conservator and no family involvement, NBRC signs and acts on behalf of their clients if they are clients of the NBRC
- Some patients with mild IDD consent for themselves
- Temp: use infrared thermometer when possible
- BP: consider wrist BP cuffs (more comfortable)
- don't assume an elevated BP is correct in setting of agitation/anxiety
- home BP checks may be more accurate
- Weights: getting accurate weights (especially for wheelchair bound) can be challenging, use table weights if available (they have at Dutton)
- Pts with IDD tend to be on multiple meds with constipating side effects (antipsychotics, seizure meds). They also may have poor PO intake, low fiber diet, sedentary lifestyle
- Underrecognized and undertreated chronic constipation
- Some people with IDD have neuromuscular dysfunction due to their underlying condition (e.g. CP)
- What should you do about it?
- Ask patients and caregivers about stooling at every visit
- Insist upon daily bowel care (not PRN only)
- If unclear, get KUB to assess stool burden
- pts with IDD often have dysphagia secondary to neurological impairment (e.g. CP) or medications (depakote, antipsychotics)
- neuromusclar disorders also include motility disorders, leading to more GERD/reflux
- some people with IDD have postural issues
- recurrent aspiration PNA causes scarring with reduce lung volumes, actually leading to a special type of COPD
- feeding tubes do NOT prevent all aspiration
- What should you do about it?
- instruct patients and caregivers to keep people sitting up after eating
- care with volume/quantity of feeding tube feeds
- hold formula, use pedialyte instead when sick with URI Sx (x48 of hte worst symptoms)
- use beta agonists nebs aggressively after aspiration sx
- consider ABI vests (if can tolerate)
- can use guaifenisin to thin secretions if aspiration event
- early warning signs are key: know the patient (e.g. "quieter than usual", decreased appetite, "just not themselves", weakness may show up as exaggerated baseline neuro issues
- understand patient hx and risk factors (e.g. recurrent aspiration, UTIs, gallstones, SBO)
- uncontrolled seizures can lead to sudden epilepsy death, aspiration PNA, other injury
- epilepsy: there is in epilepsy specialist (for IDD and not) at Dutton
- many new seizure meds that have less monitoring and less toxicity (e.g. keppra, pharmaceutical grade CBD=Epidolex)
- Vagal Nerve Stimulators (VNS) can improve qol, especially after 2-3 unsuccessful seizure meds
- Slow medicine: use serial exams, don't try to get it all done at once
- Train caregivers to look out for signs of illness
- Agitation may be a sign of communication or physical distress (e.g. pain)
- don't forget neurogenic bladder, BPH in older men!
- consider emotional sources: frustration, inability to communicate, abuse
- Dual diagnosis is common (depression, anxiety, psychosis, ADHD)
- Dementia (particularly in DS) very high incidence
- Always send dislodged J tube to ER
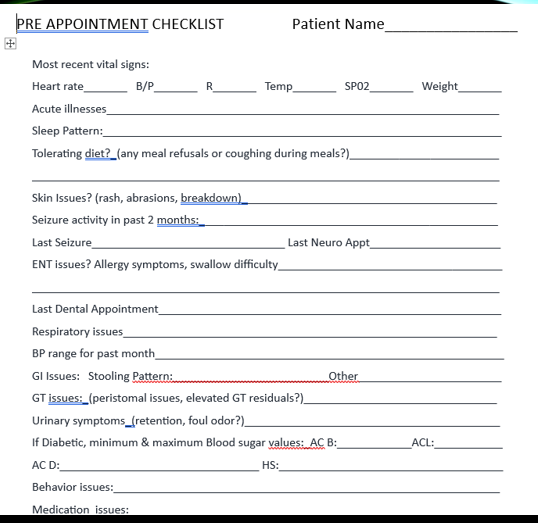
- Health passport and pre-appointment checklist available on IDD orderset in ECW at SRCH (see images below)
- primary care IDD co-management (Dr. French, Dr. Camarata, Brittney English FNP)
- dental care (including sedation)
- podiatry
- neurology/epilepsy (Dr. Rowena Korobkin)
- general surgery (Dr. Michael Bozuk)
- psych, behavioral health, including psych tech (Dr, Tract Jones, Mark Hecker PT)




No comments:
Post a Comment