Here are Dr. Smith's tips:
Examination of the patient with knee pain
- Gait: ask patient to walk across the room and back (look for flat feet, among other things)
- Alignment: look at legs standing (varus=bow-legged, valgus= knock-kneed)
- Range of motion: looking for difference in joint ROM compared to the OTHER knee
- Joint line tenderness
- Effusion?
- Check hips (seated internal rotation-- this is to be sure you are not missing a primary hip problem)
Imaging for a patient with knee pain
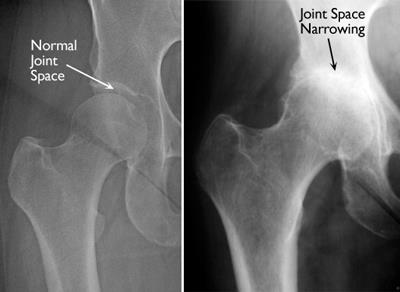
- X-ray is the imaging modality of choice for osteoarthritis
- For knees, always get standing AP views of BOTH knees, lateral view of BOTH knees
- For hips, always get images of BOTH hips
- Remember, sometimes the xray may be incongruent with the patient's symptoms (e.g. both hips look severe, but patient only has pain on one side)

- If you look at the x-ray (ideally look at the image WITH the patient), you are looking to characterize mild-moderate arthritis (some joint space narrowing, small spurs) vs moderate-severe changes (bone on bone, bone sclerosis, sub-chondral cysts)
- Do NOT order an MRI before an xray because. . .guess what?
- If there is evidence of DJD on the xrays, you don't actually NEED an MRI!
- You have made the diagnosis and can start the treatment.
What about arthritis and meniscus tears?
- All knees with arthritis have meniscus tears
- The pain is almost always due to the arthritis, and arthroscopy (meniscectomy) doesn't help, with very rare exception
Treatment of knee and hip arthritis
- Don't forget to explain the diagnosis: "you have arthritis in the right knee""
- Make the distinction between mild-moderate and mod-severe "You have severe arthritis in your right knee"
- Dr. Smith recommends this analogy: The protective coating on the ends of the bones has worn away, like the tread on a tire. You are now on the steel belt (mild-mod arthritis) or the rim (mod-severe arthritis)
What can patients do?
- Relative rest/modified activity: many patients love to walk and run, but probably best to switch to swimming and/or stationary cycling (then they can keep up their aerobic exercise)
- OTC meds: NSAIDs (if not contraindicated, be sure to check labs, particularly for SCr), acetaminophen, glucosamine, fish oil, CBD. Avoid opiates.
- Physical therapy, (it's good idea to do some PT before knee or hip replacement, but remember Medicare only covers 18 visits/year, don't use them all up if a patient is going to get surgery)
- Steroid injection: if the injection works and lasts a few months, okay to repeat (up to 4 times/year) for severe pain, but if only helps for a week, then probably not worth it
- hips done by radiology at the hospital
- Not great evidence for hyaluronic acide injections (costs $500-1000, usually cash)
- Knee bracing not indicated, some patients feel more comfortable/supported in a neoprene knee sleeve. This isn't helpful but if it makes them feel better is fine
When is a patient ready for surgery ?
- When they are ready.
- When you might consider them ready?
- If they are having sleep issues due to pain
- If they have significantly modified their activity and are missing out on things they would normally enjoy because of their pain
- There is no lower or upper limit of age for hip or knee replacements. It's really the severity of the arthritis and their degree of illness/wellness.
Surgical Preoperative Optimization
- Anemia, goal Hb>12 reduces transfusion risk (perioperative transfusions actually increase the risk of infection and LOS)
- Smoking, goal quit at least 6 weeks before surgery, including ALL nicotine products (nicotine affects wound healing and infection risk)
- Diabetes, goal <7.5 (infection risk)
- Obesity, goal BMI <30, most surgeons won't operate if BMI>40
- Malnutrition (albumin >3,5)
- And more!
- immune status, hypothyroid, low vitamin D, CV disease, ASA class, opiates, CKD, sleep apnea, psychiatric illness, social factors, deconditioning



No comments:
Post a Comment