Many thanks to Dr. Neema Pourtaheri of Santa Rosa Orthopedics for his presentation, Evaluation and Treatment of Shoulder Pain
A recording of his presentation is available HERE.
Shoulder pain is a very frequent complaint in primary care, can be broken down into several common categories
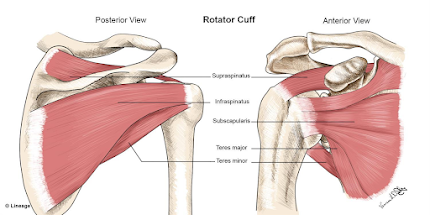
1) Rotator cuff and Proximal Biceps Tears (partial vs. full thickness, acute/traumatic vs. chronic/degenerative)
- the rotator cuff is responsible for shoulder rotation, stabilization, and arm elevation
- the rotator cuff holds the head of the humerus in the small shallow glenoid
- rotator cuff muscles: supraspinatous, infraspinatous, teres minor, subscapularis
- rotator cuff tear very common, 2 million people in US/year
- important history in your diagnosis of rotator cuff injury: usually in dominant arm, age >40 years, pain worse at night, interferes with sleep, weakness with rotation and lifting, unable to do daily tasks (e.g. combing hair, putting on shirt)
- Exam
- drop arm sign (supraspinatus)
- bear hug test (subscapularis)
- external rotation lag sign (infraspinatus)
- horn blower sign (teres minor)
- acute traumatic usually occurs in setting of fall, trauma, significant amount of force (particularly in young patients)
- chronic is degenerative, gradual onset, repetitive stress injury, occurs often in dominant arm, often as a result of bone spurs rubbing
- >40% of people >65 have chronic rotator cuff tear
- rotator cuff tears DO progress with time
- full thickness tendon tears progress more rapidly
- larger tears progress more quickly as well
- Non-surgical management: activity modification, NSAID, cortisone?? (controversial, Dr. Pourtaheri doesn't recommend steroid injection for rotator cuff injury), PT helps with strength and pain, doesn't fix the tear, work on strengthening other tendons
- All acute traumatic tears in people <60 should be fixed
- "old tendons are not fixable" (no atrophy on MRI)
- Shoulder arthroscopy: small incisions w/camera, nerve block for pain
- Rotator cuff repair in correct candidates have 95% success rate (in terms of pain, function), improved shoulder strength and prevent tears from progressing
- Post op course: 6 weeks in sling, 3 month limited lifting, PT
2) Impingement/Bursitis
- inflammation of the bursa, usually due to overuse (overhead activity), sometimes trauma
- pain exacerbated with activity, relieved with rest/NSAIDs, immobility
- no-op treatment: activity modification, steroid injection, ice, ultrasound, PT
- arthroscopic surgery for bursitis is generally arthroscopic bursectomy w/arthroplasty on the undersurface of the acromion
- rehab is faster than rotator cuff: sling x 2 weeks, PT within 2 weeks of surgery
3) Shoulder Labrum Tear
- Labrum is fibro-cartilaginous ring that attaches to the glenoid, anchor point for gleno-humeral ligaments
- labrum is essential for shoulder stability in people <40
- in people <40 tears are usually associated with trauma or dislocation event
- in people >40, most labrum tears are physiologic and don't need treatment or surgery
- PT is best non-operative management
- Sometimes surgery is indicated for people who are young and failed PT
4) Shoulder arthritis
- >60 year old patient arthritis is a common cause of shoulder pain
- articular cartilage thins out with time, exposed bone
- X-ray: collapsed joint space, large bone spurs, thickening of subchondral
- Non operative management: NSAID, PT, steroid/cortisone injection (yes, indicated)
- PT to stretch the shoulder joint capsule (see exercises below)
- Operative tx: shoulder arthroscopy (to release joint capsule, usually in mild to mod arthritis)) and shoulder replacement
- Shoulder replacement 90% pain relief indicated for moderate-severe arthritis of gleno-humerus
- there have been significant advances in shoulder replacement techniques and technology over the last 10 years
- same day (outpatient surgery)
- 4-6 weeks immobilized in sling, PT within a week, full recovery 6 months-1 year
- two types of shoulder replacement: anatomic (intact rotator cuff) vs. reverse shoulder replacement (non anatomic)-- shoulder arthritis w/large rotator cuff tears
- in reverse, ball goes on socket side of shoulder, socket on ball side of shoulder
Final pearls:
- History and physical exam are key for assessment and diagnosis of shoulder pain
- X-rays are still always a good idea as an initial evaluation (arthritis, calcific tendonitis, acromial bone spurs, for large rotator cuff tears for decision-making for surgery)
- MRI definitively diagnose rotator cuff tears
- Role for ultrasound? In patients who cannot get MRI (e.g. pacemaker), can use for shoulder injections (ultrasound guided)
- Absolute indications for MRI in shoulder pain
- fall/acute injury with sudden onset weakness in the arm likely has an acute rotator cuff tear(to evaluate for rotator cuff tear, which should be repaired within a couple months of injury for best outcome, time sensitivite)
- if concern for biceps tendon "Popeye" arm (full thickness tear of biceps tendon)





No comments:
Post a Comment